EvergreenHealth & Premera Contract Negotiation, Patient FAQ
Following months of negotiations, EvergreenHealth and Premera have reached an agreement on a new contract, allowing EvergreenHealth to remain a participating provider in Premera insurance products.
Premera Blue Cross, EvergreenHealth Reach New Multi-Year Agreement
Mountlake Terrace and Kirkland, Wash. – Premera Blue Cross and EvergreenHealth today announced they've reached a new multi-year agreement. The new contract allows members across all Premera lines of business, including commercial, individual and Medicare Advantage, to retain in-network access at EvergreenHealth, which has facilities throughout King and Snohomish counties. Read the full press release
For our Premera patients, this means that EvergreenHealth services, providers and locations will continue accepting Premera insurance products, and you will continue to receive the same level of coverage and benefits you currently have through your Premera plan without any changes.
We know that the potential disruption in insurance coverage for our Premera patients has likely been stressful. That is why we are very pleased to announce this positive outcome, which upholds our unwavering commitment to keep you—our patients—and the community we serve as a public hospital district top of mind, always.
These FAQs help provide you with data and background about why negotiations with Premera were necessary, and how the mounting costs for supplies, labor and pharmaceuticals, and lasting impacts from the pandemic continue to put EvergreenHealth and hospitals systems across Washington into unprecedented financial crisis. Now, while our state's healthcare systems are in financial crisis, we are working to ensure all organizations that support the health of our patients, including insurance companies, are doing so responsibly and with accountability in the face of rising costs so that our hospital can remain viable for those who depend on us.
Patient FAQ
What prompted negotiations between EvergreenHealth and Premera?
EvergreenHealth and Premera were re-negotiating contract "reimbursement rates". First, it's helpful to understand what a reimbursement rate is and how these rates are established.
When a patient with insurance visits a hospital and receives care, the hospital covers the cost for the patient's services upfront, and then submits a bill to the patient's insurance company. The insurance company then reimburses, or in other words, pays the hospital back for the healthcare services that were provided to the patient. How much the insurance company reimburses the hospital for the patient's services is based on the patient's insurance plan coverage and the rate of reimbursement that is agreed upon through a contract that the hospital and insurance company enter into. These reimbursement rates are negotiated on an annual basis, and insurance companies are allowed to negotiate different rates at different hospital systems.
EvergreenHealth initiated the negotiation for fair reimbursement rates in the fall of 2022 because of two primary reasons:
- Significant Increases and Continuously Rising Costs to Provide Patient Care – Unsustainable for Hospitals to Remain Viable
- The cost of labor, basic supplies, and pharmaceuticals are sharply rising for hospitals everywhere. As a result, combined with lasting financial impacts from the pandemic, The Washington State Hospital Association recently reported that hospitals and health systems losses in Washington grew to $2.1 billion in 2022. All urban and suburban hospitals in our state incurred a loss, with only a few essential rural hospitals bucking the trend due to government support. In 2023 hospital losses continue to mount.
- EvergreenHealth is not immune. In the fourth quarter alone of 2022, EvergreenHealth incurred a $36 million loss.
- EvergreenHealth Is Committed to Seeking Fair Payment for Its Services
- Under new federal price transparency laws, more data is becoming available, which means hospitals have much greater insight into the market value of their services.
- This transparency data is publicly available information from independent sources, like RAND Corporation's Hospital Price Transparency Report.
- Now, insurance companies can be held more accountable to provide fair and similar rates for similar services to ensure hospitals are able to maintain services and keep their doors open to their communities.
- Fairly addressing this issue is imperative now more than ever as hospitals across our state are experiencing financial crisis and we continue to weather severe aftershocks from the pandemic, exacerbated by the current economic state and exponential increases in the cost of labor, supplies, and pharmaceuticals. Learn more below.
Back to top
Does the reimbursement payment insurance companies pay hospitals cover the actual cost of care? Why is EvergreenHealth seeking a higher reimbursement rate?
In some cases, the reimbursement rate that the insurance company pays the hospital for services rendered is below what the actual cost of patient care totals for the hospital or below what other insurance companies would pay for the same service. This means that for some services, hospitals are paid less than is adequate or needed for that care.
Due to the sharp rise in cost for hospitals to provide care, and the need to receive fair payment, now more than ever it was important to receive an increase in reimbursement to more closely align with the increasing costs to care for patients.
Back to top
In general, what outside factors influence reimbursement rates?
Because of the volatile nature of fluctuating costs in healthcare supplies, labor, and pharmaceuticals, it is often necessary for hospital systems to renegotiate the reimbursement rate from insurance companies so that payment from the insurance companies actually covers the real costs of providing care – at least for most services – to ensure the hospital can remain viable. Like any organization, even public hospital districts like EvergreenHealth must take in enough revenue to cover expenses.
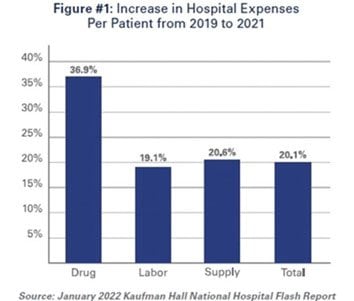
Right now, hospitals across the state and nation are experiencing unprecedented financial losses due to many complex factors that are out of hospital systems' control – namely, significant increases in labor, supply, and pharmaceutical costs. According to a January 2022 Kaufman Hall national hospital report, the cost of labor has increased by 19.1%, supply costs by 20.6%, and pharmaceutical costs by 36.9%.
To further illustrate financial circumstances in our state and the need for increased reimbursement, the Washington State Hospital Association reported that hospitals and health systems losses in Washington grew to $2.1 billion in 2022 – and losses continue to mount for hospitals.
Learn more about the financial crisis Washington state hospitals are experiencing from Washington State Hospital Association.
Now, during a time that our state's healthcare systems are in financial crisis, we are working to ensure all organizations that support the health of our patients, including insurance providers, are doing so responsibly and with accountability in the face of rising costs.
Back to top
Our Commitment to You and Everyone We Serve
Foremost, we are relieved to have reached a fair agreement without any impact to our Premera patients. Please know that this negotiation was not about increasing revenue for the hospital - it was solely about covering the exponential increases in what it costs to provide healthcare and holding Premera and all partners accountable to pay fair rates which ultimately, allows EvergreenHealth and all hospitals to continue to provide critical services to the community.
As a public hospital district, it is an inherent part of our mission to provide access to high-quality, high-value care for everyone we serve in our district. At EvergreenHealth, that means hiring top clinical experts and providing the best possible outcomes at an affordable cost – which is illustrated by our recognition as at Top 50 hospital in clinical excellence by Healthgrades, and our rank as second in the state by the Lown Institute for high-value care. Maintaining and sustaining viable access for our patients is our only goal.
Back to top