Approximately 25 million Americans suffer from venous disease, a condition that often results in varicose veins and other painful symptoms. This disease can have a tremendous effect on a person’s lifestyle. At EvergreenHealth Surgical Care we perform the VNUS closure procedure, the latest technology using radio frequency ablation (RFA) closure of the greater saphenous vein to treat this condition and improve our patient’s quality of life.
The VNUS Closure is a clinically proven, minimally invasive procedure that treats varicose veins and their underlying cause, venous reflux, with little or no pain. This procedure allows us to offer a novel alternative to vein stripping. Typically,VNUS closure patients can walk away from the procedure and be back to everyday activities within a day.
EvergreenHealth Surgical Care offers many options for vascular surgeries. The following are our main areas of service available:
Abdominal aortic aneurysm repair
Indication
To prevent death from rupture of the aneurysm.
Preoperative evaluation
First your doctor performs a complete history and physical exam. Then the initial test to detect and measure the aneurysm is either an ultrasound (Aortic ultrasound ) or a CAT scan (computed tomography) of the aorta. If aneurysm repair is to be undertaken, further anatomic information is obtained with an aortogram (X-ray study of the aorta using dye). A stress test may be ordered as well. This is to be sure that the heart is strong enough to withstand surgery.
 Procedure
Procedure
The aneurysm is replaced with an artificial blood vessel made from specially woven Dacron material.
Length of stay
One to three days in the intensive care unit (ICU) followed by 4 to 6 days in a regular room.
Recovery
4 to 6 weeks with no driving for two weeks and no heavy lifting (over 15 lbs.) for 6 weeks.
Aorto-femoral bypass
Indication
To improve the circulation to the legs in select patients with peripheral vascular disease.
Preoperative evaluation
First your doctor performs a complete history and physical exam. Then the initial study is a lower extremity arterial exam, usually performed before and after treadmill exercise. Further information about the location of blockages in the abdominal or leg vessels is obtained with an arteriogram. This X-ray study of the arteries in the abdomen and leg uses dye to allow the blockages to be seen and photographed. A stress test may be ordered as well. This is to be sure that the heart is strong enough to withstand surgery.
 Procedure
Procedure
An upside-down "Y" shaped graft (artificial blood vessel made of Dacron) is used to bring circulation from above the blockages (in the abdominal or leg arteries) down to the femoral arteries in the groin.
Length of stay
One to three day stay in the intensive care unit (ICU) followed by four to six days in a regular room.
Recovery
Four to six weeks with no driving for 10-to-14 days and no heavy lifting (more than 15 lbs.) for six weeks.
Carotid endarterectomy
Indication
To prevent a stroke in patients with narrowed carotid arteries.
Preoperative evaluation
First, your doctor performs a complete history and physical exam, then the degree of narrowing in the carotid arteries is determined using an ultrasound test (Carotid duplex) . A carotid arteriogram may be ordered to further define the anatomy in some patients. An arteriogram is a dye test much like a cardiac catheterization. However, during a carotid angiogram the dye is injected into the neck arteries instead of the heart vessels.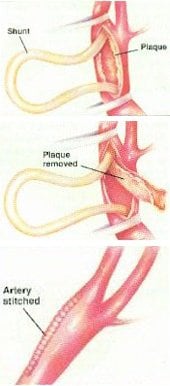
Procedure
The carotid artery is exposed through an incision on the side of the neck. The artery is clamped above and below where the narrowing is located. The flow of blood to the brain is maintained with the use of a specialized shunt (tube) that carries blood to the brain during the procedure. The diseased material narrowing the artery is removed. The artery is then sewn closed.
Length of stay
Overnight
Recovery
1-2 Weeks with no driving for the first two weeks after surgery.
Dialysis access placement
Indication
To provide an access site to perform dialysis.
Preoperative evaluation
First your doctor performs a complete history and physical exam with attention to finding a good vein in the forearm.

Procedure
The "best" vein available in the arm is located and a connection is made to a nearby artery. This connection is either made directly or with an intervening plastic graft which is tunneled under the skin. This provides a high flow circuit to "plug into" to perform the dialysis treatment.
Length of stay
This is an outpatient procedure.
Recovery
The arm should be elevated for the first day or two (longer if swelling persists). There are otherwise essentially no restrictions after surgery.
Lower extremity revascularization
Indication
Claudication (pain in the legs from walking), ischemic rest pain, or non-healing wounds.
 Preoperative evaluation
Preoperative evaluation
First your doctor performs a complete history and physical, including a careful examination of the pulses in the legs. The next study generally obtained is a lower extremity arterial Doppler exam. This more precisely quantifies the amount of circulation to the legs. If it is felt a revascularization procedure is needed, an arteriogram is then performed, usually in the radiology department at the hospital.
Procedure
A bypass is performed to bring blood flow around the blocked arteries in the leg. The bypass can be made with the patient’s own vein or with an artificial (plastic) bypass graft.
Length of stay
Three to five days.
Recovery
Two to four weeks.
Renal artery (kidney) revascularization
Indication
To lower blood pressure in select patients with very high (diastolic BP > 110) blood pressure and to preserve renal function (prevent kidney failure requiring dialysis) when the arteries to the kidneys are found to have narrowings.
Preoperative evaluation
First your doctor performs a complete history and physical exam. Then the initial study ordered may be a Renal artery duplex examination or a nuclear medicine scan. Ultimately, a renal artery arteriogram is required to further define the narrowings in the renal arteries.
Procedure
Depending on the patient’s anatomy and overall health, several options may be considered. The narrowed renal arteries can be opened with a balloon procedure in carefully selected cases. In other patients a bypass is a more durable option. A bypass can be performed from a nearby artery to beyond the narrowed area of the renal artery.
Length of stay
One to three day stay in the intensive care unit (ICU) followed by four to six days in a regular room.
Recovery
Four to six weeks with no driving for 10-14 days and no heavy lifting (over 15 lbs.) for six weeks.
Vein stripping
Indication
To remove large (greater than 1/8 inch in diameter), symptomatic varicose veins. This surgery is usually reserved for patients who have failed to respond well to the use of compression stockings.
Procedure
Just before going back for surgery, with the patient standing, the veins to be removed are marked with ink. After anesthesia is given, small incisions (less than ¼ inch) are made next to each varicose vein. The veins are then extracted with a small hook, the excess length excised, and the ends tied off. The incisions are small enough that they can be closed with "steri-strips" and no sutures are required.
Length of stay
Outpatient or occasionally overnight.
Recovery
Treated legs should be elevated initially to minimize swelling and bruising. The recovery is otherwise rapid.
Vena cava filter placement
Indication
To prevent pulmonary embolism in the presence of deep venous thrombosis (blood clots in the large deep veins of the legs that could then travel to the lungs or heart.)
Preoperative evaluation
After a focused history and physical exam, a venous duplex examination is reviewed to look for blood clots in the leg veins.
 Procedure
Procedure
The femoral vein (large leg vein located in the groin) has a hollow wire, called a catheter, inserted into it. Dye is injected through the catheter and an x-ray picture of the inferior vena cava (the largest vein in the body, which leads directly to the heart) is taken. After the patients anatomy is demonstrated on the x-ray, a small umbrella shaped metal device (the filter) is placed into the vena cava to catch any traveling blood clots before they can reach the heart or lungs.
Length of stay
The skin puncture site that the catheter was placed through is observed for two hours after which normal activity may be resumed.
Recovery
There are otherwise no restrictions and an inpatient stay is not required unless other treatments are required (for instance, the administration of blood thinners).
VNUS closure procedure (varicose veins)
 If you experience discomfort, swelling and varicose veins in your legs, you may be suffering from superficial venous reflux disease. Venous reflux or venous insufficiency develops when the valves that usually keep blood flowing out of your legs become damaged or diseased.
If you experience discomfort, swelling and varicose veins in your legs, you may be suffering from superficial venous reflux disease. Venous reflux or venous insufficiency develops when the valves that usually keep blood flowing out of your legs become damaged or diseased.
Traditionally, you would undergo vein stripping surgery to remove the vein from your leg. Now, you can be treated with the Closure procedure - a minimally invasive alternative that closes the diseased vein instead.
The closure procedure
The Closure procedure can be performed on an outpatient basis using either local or general anesthesia in which the physician numbs the leg before treatment. The procedure consists of four principal steps:
Map the saphenous vein
A typical procedure begins with noninvasive ultrasound imaging of the diseased vein to trace its location. This allows the physician to determine the site where the Closure catheter will be inserted and to mark the desired position of the catheter tip to begin treatment.
Insert the Closure catheter
After the physician accesses the saphenous vein, the Closure catheter is inserted into the vein and advanced to the uppermost segment of the vein. The physician then typically injects a volume of dilute anesthetic fluid into the area surrounding the vein. This numbs the leg, helps squeeze blood out of the vein and provides a fluid layer outside the vein to protect surrounding tissue from heat once the catheter starts delivering RF energy.
Saline is then slowly infused into the vein from the tip of the catheter to further create a near-bloodless field inside the vein, allowing the catheter to preferentially heat the vein wall, rather than the blood.
Deliver RF energy and withdraw catheter
Noninvasive ultrasound is used to confirm the catheter tip position and the physician then activates the RF generator, causing the electrodes at the tip of the catheter to heat the vein wall to a target temperature of typically 85 degrees Centigrade or 185 degrees Fahrenheit. As the vein wall is heated, the vein shrinks and the catheter is gradually withdrawn. During catheter pullback, which typically occurs over 15 to 18 minutes, the RF generator regularly adjusts the power level to maintain target temperature to effectively shrink collagen in the vein wall and close the vein over an extended length.
Confirm closing of vein
After treatment, ultrasound imaging is used to confirm closing of the vein. If a portion of the vein is not closed, the catheter can be reinserted and energy reapplied. After the procedure, the narrowed vein gradually becomes fibrous, sealing the interior of the vein walls and naturally redirecting blood flow to healthy veins. Experienced physicians often complete the procedure in 45 to 60 minutes.
Recovery
Patients who undergo the Closure procedure typically resume normal activities within a day. 98 percent of patients who have undergone the Closure procedure are willing to recommend it to a friend or family member.
Physicians generally instruct their patients to walk regularly for several days after the Closure procedure and return within 72 hours for an ultrasound examination. Physicians may prescribe compression stockings to be worn for several days or weeks after the procedure. Compression stockings are prescribed as a routine item for vein procedures with the goal of enhancing patient comfort in the initial days after treatment.
There is usually minimal or no scarring, bruising or swelling.